
Tricks to rapidly terminate episodes of cataplexy in narcolepsy. International classification of sleep disorders-third edition (ICSD-3). 1974 31:255–61.Īmerican Academy of Sleep Medicine.
Behavioural and neurophysiological correlates of human cataplexy: a video-polygraphic study. Vetrugno R, D'Angelo R, Moghadam KK, Vandi S, Franceschini C, Mignot E, et al. Overview of the clinical features of cataplexy in adults. The clinical features of cataplexy: a questionnaire study in narcolepsy patients with and without hypocretin-1 deficiency. Overeem S, van Nues SJ, van der Zande WL, Donjacour CE, van Mierlo P, Lammers GJ.Clinical, behavioural and polysomnographic correlates of cataplexy in patients with narcolepsy/cataplexy. Mattarozzi K, Bellucci C, Campi C, Cipolli C, Ferri R, Franceschini C, et al. Effects of startle and laughter in cataplectic subjects: a neurophysiological study between attacks. Lammers GJ, Overeem S, Tijssen MA, Van Dijk JG. Cataplexy-clinical aspects, pathophysiology and management strategy. 2015 373:2654–62.ĭauvilliers Y, Siegel JM, Lopez R, Torontali ZA, Peever JH. Diagnostic delay in narcolepsy type 1: combining the patients' and the doctors' perspectives. Taddei RN, Werth E, Poryazova R, Baumann CR, Valko PO. Papers of particular interest, published recently, have been highlighted as: ĭauvilliers Y, Arnulf I, Mignot E. Importantly, management also needs to involve sleep hygiene advice, safety measures whenever applicable and guidance with regard to the social sequelae of cataplexy.
Symptomatic treatment is possible with antidepressants and sodium oxybate.
#Examples of cataplexy series#
Over time, these severe symptoms evolve to the milder adult phenotype, and this pattern is crucial to recognize when assessing the outcome of uncontrolled case series with potential treatments such as immunomodulation. Cataplexy shows remarkable differences in childhood compared to adults, with profound facial hypotonia and complex active motor phenomena.
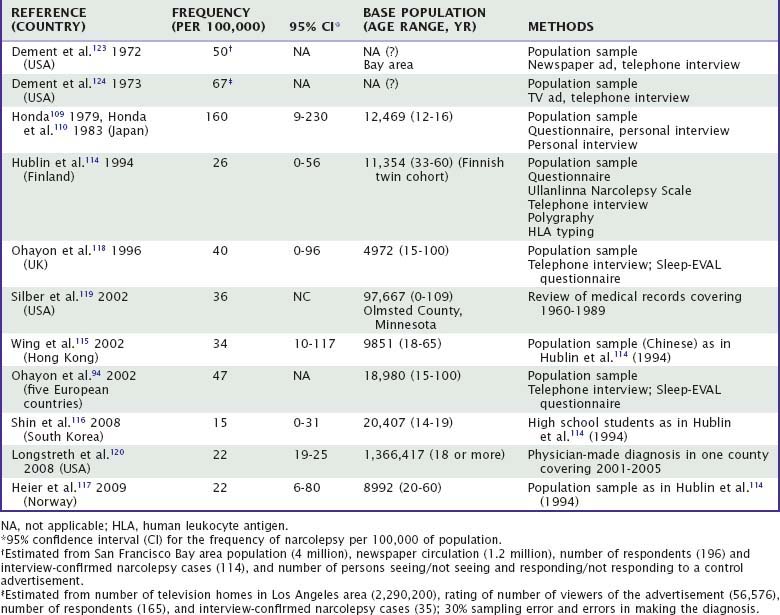
Currently, the diagnosis of cataplexy is made almost solely on clinical grounds, based on history taking and (home) videos. Childhood narcolepsy, with its profound facial hypotonia, can be confused with neuromuscular disorders, and the active motor phenomenona resemble those found in childhood movement disorders such as Sydenham’s chorea. They can be differentiated from cataplexy using thorough history taking, supplemented with (home)video recordings whenever possible. Cataplexy mimics include syncope, epilepsy, hyperekplexia, drop attacks and pseudocataplexy. Next to narcolepsy, cataplexy can sometimes be caused by other diseases, such as Niemann-Pick type C, Prader Willi Syndrome, or lesions in the hypothalamic or pontomedullary region. Moreover, childhood cataplexy differs from the presentation in adults, with a prominent facial involvement, already evident without clear emotional triggers (‘cataplectic facies’) and ‘active’ motor phenomena especially of the tongue and perioral muscles. The expression of cataplexy varies widely, from partial episodes affecting only the neck muscles to generalized attacks leading to falls. Although cataplexy is rare, its recognition is important as in most cases, it leads to a diagnosis of narcolepsy, a disorder that still takes a median of 9 years to be diagnosed. This review describes the diagnosis and management of cataplexy: attacks of bilateral loss of muscle tone, triggered by emotions and with preserved consciousness.


 0 kommentar(er)
0 kommentar(er)
